Cortisone injections are commonly used for many joint and tendon musculoskeletal conditions. People with diabetes are more prone to side effects from cortisone injections, so they should be more careful when considering these injections. Cortisone injection and diabetes: what should you know to ensure you make the right decision to have one?
Why are we concerned about diabetics?
Diabetes means your ability to metabolise glucose is reduced, increasing blood glucose levels.
Elevated blood glucose levels increase the risk of developing common musculoskeletal conditions and make treating these conditions more difficult:
- Frozen shoulder
- Trigger finger
- Achilles Tendonitis
- Knee and hip osteoarthritis
- Carpal tunnel syndrome
Moreover, cortisone injections are commonly used to treat these musculoskeletal conditions but are more risky when given to people with diabetes.
Specific risks associated with cortisone injection and diabetes
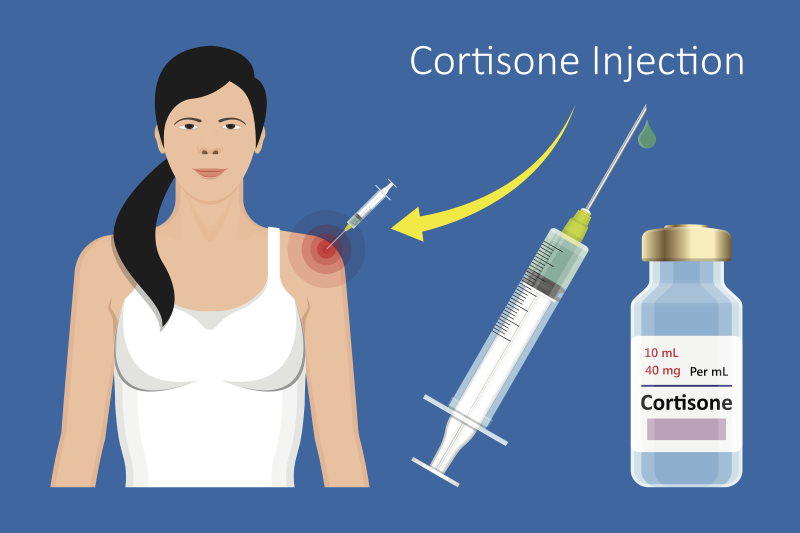
We know that cortisone increases blood glucose levels, which are higher and stay elevated for longer in people with diabetes. A few studies outline the problem with raised sugar levels after a cortisone injection:
- One study of type 2 diabetics after a shoulder cortisone injection found that sugar levels stayed elevated for three days but normalised from day four onwards. Only 10% of these patients had high sugar levels, but none needed extra tablets or insulin.
- Another study after a shoulder injection found that well-controlled diabetics had elevated sugar levels until Day 8, but poorly controlled diabetics or those on insulin had much higher glucose levels that remained elevated for more than ten days.
- Cortisone injections into the hand in people with diabetes found an increase in sugar levels for 1-2 days. These levels were higher and lasted longer in insulin-dependent diabetics.
Other factors associated with raised sugar levels after a cortisone shot are the type and dose of cortisone used. Generally, we recommend a more conservative approach in people with diabetes by using a slightly lower amount of less potent cortisone (such as Depo-medrol rather than more potent Triamcinolone).
In addition, we know that people with diabetes have lower immune function. So, people with diabetes are at an increased risk of infection following a cortisone injection.
How to manage increased sugar levels

In general, people with diabetes should be aware of the risk of a transient increase in blood glucose after a cortisone shot. This risk of elevated sugar levels is more common in poorly controlled or insulin-dependent diabetics.
Ensure you tell your doctor about your diabetes, including recent sugar levels and HBA1C and oral medication or insulin dose.
Usually, elevated sugar levels are transient and normalise after a few days. However, you should take the following precautions if you have diabetes and are considering a cortisone injection:
- Consider postponing the injeciton if your sugar levels are unstable or HBA1C is greater than 7%.
- Monitor your sugar levels closely (at least a few times daily) for five days after a cortisone shot. If you have unstable diabetes or use insulin, you should monitor for ten days.
- Start monitoring about 6 hours after the cortisone shot.
- If your sugar levels are high, consider taking more insulin or oral medication. If they remain very high despite a medication change, you should speak to your GP or visit your nearest emergency department.
Other frequently asked questions about cortisone injections and diabetes:
How can I lower my sugar levels after a cortisone shot?
It would be best to diet carefully and exercise more (although you should speak to your doctor about post-injection activity). However, generally, we suggest you increase your oral or insulin medication to counteract the effect of a cortisone shot.
Do people with diabetes respond as well to cortisone injections and other treatments in common musculoskeletal conditions?
As a rule, people with diabetes take longer for pain and function to improve with common conditions such as frozen shoulder and Achilles tendonitis. But having diabetes doesn’t mean you have to live with your condition.
A final word from Sportdoctorlondon regarding cortisone injection and diabetes
Ensure you tell your doctor if you have diabetes before you have a cortisone shot. In general, blood sugar levels remain elevated for up to 10 days, but this depends on your level of sugar control and whether you’re on insulin.



Leave A Comment