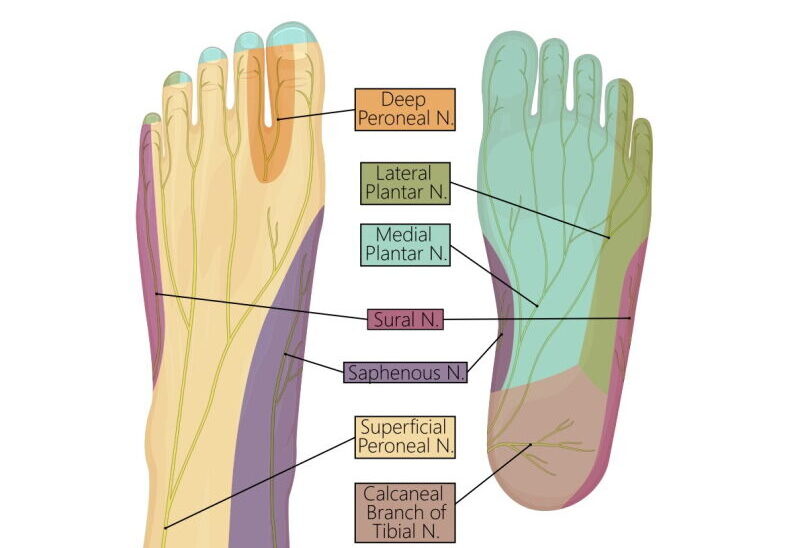
Multiple nerves supply the front, sides and back of the foot. These nerves can be pinched by joints, muscles and tendons within the foot, causing pain, numbness, and pins and needles. What are the most common causes of a pinched nerve in the foot, and how do we manage these conditions?
Common causes of a pinched nerve in foot
Pinched nerve in the ball of the foot: is it Morton’s neuroma?

Morton’s neuroma is a thickening or swelling of the nerve between the small bones of your forefeet. We think the trapping is brought on by abnormal foot biomechanics and wearing the wrong footwear.
Generally, patients report pain at the sole, usually between the toes. Often, pain is described as a feeling of a stone in a shoe. Pain can be like an ache, sharp, or burning. Usually, excessive walking or running can cause worsening pain. Numbness or pins and needles radiating into the toes occur in some cases. Commonly, there is tenderness between the toes. In addition, a ‘Mulder’s’ click can be felt when squeezing the toes together.
It is essential to confirm a correct diagnosis with imaging. Ultrasound shows thickening and swelling of the nerve between the toes. In more complex cases, MRI is useful to rule out other causes of foot pain.
Pinched nerve in inner foot: Is it tarsal tunnel syndrome?

The tarsal tunnel is a space between the bottom of the long bone called the tibia and the inside of the Achilles tendon. A tough retinaculum covers it and contains nerves, vessels, and tendons.
Tarsal tunnel syndrome occurs when the posterior tibial nerve is compressed in the tarsal tunnel, similar to carpal tunnel syndrome in the wrist. Compression causes include a ganglion cyst, arthritis spurs, extra muscles in the inside ankle, or ankle twisting.
Symptoms of tarsal tunnel syndrome include burning or shooting pain at the inside ankle and mid-arch. Sometimes, numbness or pins and needles can occur in the inside arch.
Pinched nerve on outside of foot: Is it sural nerve entrapment?
The sural nerve starts at the outer top part of the lower leg and travels down the calf close to the Achilles tendon. It winds around the outer part of the ankle to end at the outer part of the foot. It provides sensation (such as light touch) from the outer part of the lower leg to the outer part of the heel, ankle and foot.
Sural nerve damage leads to pain in the outer lower leg. Generally, the pain is burning but could also be sharp and shooting. Sometimes, pain radiates down into the outer part of the foot or up into the top part of the calf. Sural nerve pain is usually present at rest and is worsened by activity such as fast walking or running. Also, sitting or driving can worsen symptoms by increasing the tension on the sural nerve. People with sural nerve irritation are sensitive to touch at the outer part of the calf and lower leg. Tapping the nerve at the trapping site will often cause a sharp. Your doctor will examine your calf and foot for evidence of sensitivity along the sural nerve. Other helpful tests include neural stretching tests such as slump or straight leg raise tests.
Investigations can help diagnose sural nerve pain. MRI scan might show inflammation of the nerve at the site of damage. However, most causes of sural nerve pain don’t demonstrate clear signs of inflammation and may be reported as normal. Generally, ultrasound is more useful as you can carefully follow the course of the nerve from the calf, looking for signs of nerve inflammation or trapping. Usually, nerve damage on ultrasound is seen as sudden nerve thickening at the trapping site.
Pinched nerve in the heel: is it Baxter’s nerve entrapment?
The Baxter’s nerve is a tiny nerve from a larger plantar nerve inside the ankle. This little nerve supplies the foot’s small muscles and sensation to the heel.
Baxter’s nerve entrapment presents similarly to plantar fasciitis, but there are a few differences. Firstly, people describe sharp or burning pain inside the heel. Sometimes, the pain moves to the arch of the foot. You may feel pins and needles and have a numb heel. Unlike plantar fasciitis, you often don’t experience morning stiffness or pain. Finally, tenderness is slightly closer to the foot’s arch than plantar fasciitis. Nevertheless, Baxter’s neuropathy is confused with plantar fasciitis, often delaying the diagnosis.
In general, imaging such as ultrasound or MRI can give clues to the diagnosis. Sometimes, you can see the thickening of the minor Baxter’s nerve on the inside of the heel. Other times, you might see a normal plantar fascia scan, increasing suspicion of nerve trapping as the cause of pain. In severe cases, nerve trapping can cause the shrinking of the muscles on the outside of the foot, best seen on MRI.
What does a pinched nerve in the foot feel like?
Generally, a pinched nerve in the foot will lead to symptoms and signs that suggest pressure on the nerve.
Common symptoms of a pinched nerve in the foot:
- Sharp stabbing pain at the site of pinching
- Burning feeling in the area of the pinching
- Numbness or pins and needles or both
- A feeling that the foot falls asleep
- Sometimes, unexplained pain may be due to a pinched nerve in the foot.
Your doctor will examine you to see if the pinched nerve is caused by local pressure in the foot or is referred from higher up, such as the spine. Pressing on the nerve at the pinching site often brings pain and other symptoms.
How to get rid of pinched nerve in foot:
Generally, we try simple measures before moving on to medications, injections and surgery.
Conservative measures
Firstly, you must avoid those activities that cause pinched nerves. For example, you should avoid running in tight-fitting shoes if you have Morton’s neuroma. Secondly, physiotherapy can help reduce the tension on pinched nerves. For example, manual therapy will help loosen the tissue around the sural nerve in the calf, and ‘neural’ stretches and glides will reduce nerve tension. Finally, massage, acupuncture, and TENS can make the nerve less sensitive.
Medication
Medication can reduce inflammation and improve nerve pain if inflammation surrounds the nerve.
Sometimes, we use oral NSAIDs such as Iburofen.
Other times, oral nerve medications are better. Generally, we use either Amitriptyline or Duloxetine. Both have pros and cons, so you should discuss these medications with your doctor.
Nerve Injections
In some cases, doctors use nerve injections, also called nerve hydrodissection, to reduce pressure on the nerves in the foot. Under ultrasound guidance, a needle is placed close to the nerve entrapment. Generally, we inject a combination of local anesthetic, sterile water and a low dose of cortisone to reduce inflammation. Common injections include Morton’s neuroma injection, tarsal tunnel injection, Baxter’s nerve injections and sural nerve hydrodossection.
These injections should be performed with ultrasound guidance to improve accuracy and effectiveness.
Surgery
Surgery to relieve nerve entrapment should only be considered in cases that have failed other treatments, including physiotherapy, medications and injections.
Final word from Sportdoctorlondon regarding a pinched nerve in the foot
A pinched nerve in the foot can cause pain in the forefoot, heel or medial arch. Generally, we suspect a pinched nerve when imaging findings are normal or patients have unexplained pain. See a sports doctor if you think you have foot pain secondary to a pinched nerve.


My second toe is swollen And red and very painful and top of my foot Swollen ,I went to Doctor And Taken Antibiotics For 10 Days No Better what to Do Jean
please see this blog on 2nd toe pain
https://sportdoctorlondon.com/second-toe-pain/
you could have another cause for a painful swollen 2nd toe (not related to infection). On example is sausage toe or dactylitis
https://sportdoctorlondon.com/inflammatory-arthritis-what-to-look-for/